New Media Medicine
| Project Infobox | |
|---|---|
| Self researcher(s) | John Moore |
| Related tools | phone |
| Related topics | Media |
Builds on project(s) |
|
| Has inspired | Projects (0) |
| Show and Tell Talk Infobox | |
|---|---|
| Featured image | 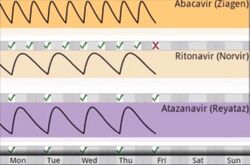
|
| Date | 2013/05/02 |
| Event name | Boston Quantified Self Health & Wellness Innovation Night |
| Slides | |
| This content was automatically imported. See here how to improve it if any information is missing or out outdated. |
New Media Medicine is a Show & Tell talk by John Moore that has been imported from the Quantified Self Show & Tell library.The talk was given on 2013/05/02 and is about Media.
Description[edit | edit source]
A description of this project as introduced by Quantified Self follows:
John Moore has a biomedical engineering background and became interested in medicine. However after practicing for years, he quit partly because he was frustrated and kind of embarrassed with the way medicine was practiced. He felt people weren't involved enough in the process. In this talk, he discusses about the work that he and his team are doing, trying to improve the healthcare experience using technology that allows patients to play a bigger role in crafting their own treatment.
Video and transcript[edit | edit source]
A transcript of this talk is below:
John Moore - New Media Medicine - Boston Q
So hopefully I’ll answer a few of those questions and ones that I’m especially interested in in are how to use data for behaviour change and then also some of the questions that were asked about how patients can really use this data with clinicians. So I came from a biomedical engineering background and then into medicine, and I quit practicing medicine partly because I was frustrated and kind of embarrassed with the way we provide medical care. People weren’t involved in the process. It was a black box. I’d see people and they’d go away and they’d come back and say well I forgot what you told me. I didn’t think it was important. I wasn’t motivated. I didn’t understand, and it was consistent and I had no tools at my disposal to change that. So that was the first part of the problem. The second part was all my buddies who were in biomedical engineering were creating great devices. They were creating all these devices that were going to measure really interesting things about your health, that have a huge potential to impact it, but I said to myself they’re going to be worthless because there is no channel for that data, not only to feed to clinicians but more importantly there weren’t channels to feed directly to patients to make it meaningful to them. So what I’m going to show you is highlighting some of the work that I’ve been doing with one of my colleagues, Scott here for the past three years and building a platform for allowing patients to really be actively involved in decisions throughout their medical care, self-reflecting upon their data, and then engaging with others on top of that data. And a big part of that is having them involved in actionable moments throughout the course of that chronic disease and the case that we look at. So what this looks like is reimagining in how decisions are made and how clinicians and patients engage with the data in the clinic. So normally it’s a very paternalistic process where someone makes a decision for the patient. The patient leaves, and they retain about five to ten percent of what was said, and then in addition to that they typically only fill medications about 70% of the time. They take them properly about half of the time. So that process of just throwing decisions at people does not stick. So what if we built this information system so that the patient is actively involved in the process, that they are moving handles, adjusting sliders. They’re experimenting with different choice architectures and try to understand the burden of testing it is with that, what the potential is for benefit but what also the potential is for detriment to their health, so that they can have agency in that decision and that they do this with family members, friends, a physician and a health coach and I’ll talk more about health coaches. But the goal is really that then these decisions are immediately synchronized out into devices in the patient’s life, cell phones, tablets, home computers. So we see a lot of that here, we see a lot of this home tracking element of different aspects of your health. But the issue here or the level of elevation of it is now it’s a decision that you’ve made with an expert in this area. It could have been a nutritionist, it could have been your primary care doc, it could have been a rehab physician. It could be something more just on the wellness slant, but you have a partner in this process. So you track these metrics over time and we make it as easy as possible to do that. And then we build architecture on top of this to do virtual visits, so we can call people really quickly to get that help. It could be that professional but it could also be a family member or a friend. And the important part is it’s not about the videos. So the video is there and it’s nice, but the really compelling part is where we can co-explore data together, so we build an architecture that is bilateral screen control, screen sharing, and screen pointing. So that when the clinicians here navigates this data points to data points and Scotts on the other end he can be involved in a real data driven discourse about his data. When you try to take IT tools and then just layer a telephone on top of them, and you have no common ground for conversation, it’s very in affective in making decisions together. But when you layer it on top of this real architecture that allows you to experiment and explore data, tweak different tools and use decisions support, then suddenly we engage in a totally different kind of partnership, that then allows us to teach competencies to patients so that eventually that we don’t need those synchronicities anymore and we can transition to a synchronized cared. So the real benefit there it’s much cheaper. We don’t need to schedule time, and it fits in a lot easier into people’s lives. And what that looks like is those same workflows just being sent over more quickly to the patient. This is not me video-conferencing with that patient but instead I’ve sent a quick message of positive reinforcement saying you did a great job in reaching that goal we set together, keep up the good work. The psychology of that experience is very powerful. Then the last bit that we get out of this platform is the ability to use awareness and other aspects of the system. So this app here when on a tablet and you dock it, it’s there all the time. So family members and friends who might be involved in partners with you and tracking an managing your disease, as they walk by they see the data as well. and it doesn’t take a voluntary act of going and launching an app and going in and digging in because you were really interested in it, instead it’s just there in passing. And it gives them the ability to then be engaged in this process without really diving into your business to the extent that people feel an invasion of privacy. And then the last part is my thesis is really around this concept as apprenticeship as a model for healthcare. So chronic disease management as I mentioned is usually paternalistic, but even in its best state when clinicians or others have really engaged in helping people tackle their problems it’s best state is just about this one given problem, getting a solution. It’s not about teaching people the skills in order to achieve that outcome on their own. So when we have tools like this what we can gradually do is the first time we make a decision that a clinicians might walk that patient through that process, articulate their thinking and then gradually allow the patient to start making that decision to the point that they’re independent, while suddenly that patient becomes a master in managing this process as well and they can start teaching other patients. So what we can start to do is build an exponentially scaling health ecosystem as opposed to our typical linear scaling health care system. They can’t keep up and it cost them an extraordinary amount of money and now we really allow people to get engaged in this process. And that’s what the last bit of the video is about that. And I’m going to take just about two more minutes to tell you a few more things. so I mentioned that my work delves into these areas of health psychology and learning science. The idea here is that health behavior change is quite complex and it’s not just about the self-reflection on the data. It’s also about really understanding and developing motivation and also having social support and social accountability. And some of the other technology techniques that we use to foster this are things like assimilation. So this is simulation for an HIV patient. It shows the number of HIV viruses in that person’s blood proportional to the last lab test that they had. The larger cells, the T-cells are part of the immune system that gets attacked by HIV; again, we just show them the number. It seems simple and what’s normally done is you see it on a chart and you see this number 5283. It doesn’t mean any sense to people. Just show it to them. if we were to look microscopically at a drop of their blood, what does it look like. And then the piece that’s the most important part of this is the fact that you need something actionable on a daily or close to daily basis that is going to effect change in the simulation. That’s how you need to engage with people, and they need to be part of some decision that happens on a regular basis. So in this case, we project this persons medication adherence onto this simulation, and what you’ll see is right now the viruses are still and they are a threat but they’re not attacking the T-cells that are floating around. And we go to our chart here which shows an actual estimate of the blood concentration of the medication, and this patient misses one medication. They see that concentration fall and they immediately see it here being translated and attacked by a virus. So now this not only becomes a much deeper, a much more potentially eliciting a visceral response from people of potentially making them even feel sick, or feel in this case scared a little bit. But when they have it in a state where they’re fully protected it’s a sense of comfort in an otherwise very scary invisible disease. So you can’t see, hear, feel, or otherwise perceive something, it’s very easy to just discount it. But suddenly when you have something like this, patients would start to come to us, we didn’t have to ask them questions anymore. They say, I saw myself getting attacked and I’m going to do something about it. so that’s a very different state than us trying to say it’s very important that you take your medication. And then we start to get patients asking about how do I prevent sharing this disease to other people, right, that’s our goal but this is a pulled mechanism because we’re engaging them. and now this becomes a common ground when we do those virtual visits and we look at it together and we’re bringing the voice of the patient to the forefront because now they have a way to really engage in it deeper. The last thing I’ll mention as I play some other simulation work that we’ve done is that this is an open source platform that we’ve developed and the purpose of making it open source is that they’re really thousands or millions of different studies that can be performed in this model of patient care. And there are studies centered around different incentive systems, different cultures or different diseases, different models of the psychology of the behavior change, different theories of progression, different models of who are the coaches. Are they clinicians, are they peer coaches are they family members. Also we want to make it open source because we know many people like you are doing work in this area. And unfortunately most efforts are completely fragmented. But if there I a common layer underneath this that people can benefit from and build on top of, hopefully this area of Quantified Self can get out of the realm of just being fragmented in individual projects that are disconnected from the actual healthcare delivery system and other interventions to being something that’s really connected throughout the whole ecosystem. And then you have your choice in how you want to engage with this.
So thanks very much.
About the presenter[edit | edit source]
John Moore gave this talk.