What Causes My Heart Rhythm Disorder
| Project Infobox | |
|---|---|
| Self researcher(s) | Mark Drangsholt |
| Related tools | Excel |
| Related topics | Cardiac, Arrythmia episodes, Activity tracking |
Builds on project(s) |
|
| Has inspired | Projects (0) |
| Show and Tell Talk Infobox | |
|---|---|
| Featured image | 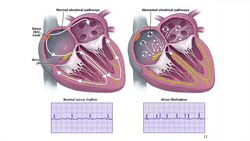
|
| Date | 2013/12/10 |
| Event name | 2013 QS Global Conference |
| Slides | |
| This content was automatically imported. See here how to improve it if any information is missing or out outdated. |
What Causes My Heart Rhythm Disorder is a Show & Tell talk by Mark Drangsholt that has been imported from the Quantified Self Show & Tell library.The talk was given on 2013/12/10 and is about Cardiac, Arrythmia episodes, and Activity tracking.
Description[edit | edit source]
A description of this project as introduced by Quantified Self follows:
Mark Drangsholt shares his heart rhythm disorder and discoveries using QS self-tracking methods.
Video and transcript[edit | edit source]
A transcript of this talk is below:
Mark Drangsholt - Conference 2013
I’m a professor and Chair of medicine at the University of Washington. My Ph.D. is in epidemiology and I teach evidence-based medicine. And what I’m going to talk about today is out of my clinical area, and it’s my story about my heart rhythm disorder. So the story starts, I just graduated from high school and I was playing tennis, and I had a sudden onset of this rapid, uncontrollable heartbeat. My heartbeat went from 100 beats per minute to about 225 and they lasted for about five minutes. And you know, understandably, I was pretty concerned. Went to a physician, a stern looking physician and he says you have paroxysmal Atrial Tachycardia, you must stop drinking coke right away. This may get worse, and you may need to take medications, and that was it. Then over the next essentially 15 to 20 years, I raced bicycles, triathlon. These events would happen, but I got used to them. They’re still a little scary, but they happen about two or three times a month, and I knew they would stop after a few minutes. Then I got married, started a family, stopped cycling and I gained 35 pounds. My heart rhythm problem was the same thankfully, but I developed high blood pressure. So my cardiologist, who is really outstanding, he gave me six months and he said, look, you have to start taking medications right now. So I was 145/105-110, which is pretty high blood pressure, and I said give me six months. I’m going to start cycling again, I don’t want to take medications yet. So then I tracked myself, it’s the first thing I really tracked and I lost a pound a week. And these embarrassing photos, the black one is because I didn’t actually have the nerve to be taking a picture of myself when I weighed 205 pounds. You can see my daughter is in the middle picture watching me here. But then I was able to lose 35 pounds over about an eight-month period. And this was how I did it. I began cycling a few days later. I change my diet, usually one item at a time. I weighed myself every day, which at the time it was strongly advised against, but now science shows that valuable. I signed up for a long distance cycling event on a tandem called RAMROD, right around Mount Rainier one-day, which is a 150 mile ride. And I made this really a lifelong commitment to a healthy lifestyle at that time in 2000 that I’ve kept to this day. So one of my big goals then was that my brother is on the back of this tandem and I’m on the front, and you can see the profile of this ride around Mount Rainier, and it has to mountain passes and 10,000 feet of climbing. And so the impetus was to lose the weight because I couldn’t weigh 205 pounds, I had to be light. Because not only did I have to be a strong cyclist but I had to be light enough to go over these mountains and also not to slow down my brother, who was counting on me. So it worked really well for me. But then, at a research meeting in 2002, just about a year later the first time in my life I thought I was going to die. I was at the back of a conference room, just like over here and I had already given a talk the day before. But I had this feeling that my heart had stopped for about five seconds, and then I had this terrible irregular beat, and I thought maybe this is what defib or vtac is like and I started greying out. And I really thought I was going to die, and instead of kind of raising my hand like you might think you might try to call for someone to help you, it was exactly the opposite. And I just sort of slump down and thought about my family, and I thought that was about it. And as it turned out, I was really lucky and I thought well I have to go to the emergency room, it stopped after five minutes, and one of my colleagues is an internest, and she heard the story and she says Mark, I think you have atrial fibrillation, and you’re probably okay and you don’t have to go into the ER but you should go and see your cardiologist as soon as you get back tomorrow to Seattle. And so that’s what I did then. So a little bit of background, some of the tachycardia, or a heartbeat of greater than 100 beats per minute, there’s parosxymsal supraventricular tachycardia, which is what I have, that is relatively benign. Something called atrial flutter, which is relatively benign. Atrial fibrillation, which can cause strokes and heart failure and it can be very dangerous. And then there’s many things, but just to name one, Wolff-Parkinson-White syndrome, which can cause sudden cardiac death. So part of the cardiologist then is they are trying to rule out the really dangerous disorders from the ones that aren’t really dangerous. So I went in and saw my cardiologist, he asked me a million questions, and at that point, I realized that even though this is a Holter monitor here that was placed on me and I had to do this several times, and they are able to record, some of them with ECG which is really powerful. Still, the history is important in cardiology, and I didn’t know a lot of the answers that my cardiologist asked me. So at one point I decided that I really needed to start to pay attention to all the information, and to start describing events, measuring triggers, and avoiding them to see if I could decrease these unpleasant and dangerous events. And I would get this terrible choking feeling with this atrial fibrillation, and it really felt like somebody was strangling me. So really simple, I started keeping track of the number of episodes, and how long they lasted, the heart rate onset and offset, time of day etc. and I could start seeing some patterns, then that I had actually maybe the three different kinds of arrhythmias. So the first thing that I did then was to try to categorize the kind of arrhythmia. And the one that was really dramatic was like I had in San Diego in 2002 with the terrible choking feeling, the irregular heartbeat, completely irregular. I had this sense of an impending doom. I was very lightheaded, and then I had a feeling that when one was coming on, a prodrone. So I would get sometimes up to 5, 10 minutes feeling like it was going to happen before it would happen. And they would last from anywhere from two minutes all the way up to 30 minutes. And then I had this other one that was rapid and irregular, like I had had since I had been playing tennis when I was aged 18, and it really wasn’t that bad, and then there was one that was a little bit in between these two. So what I did then was very simple. I just created an Excel table with all the episodes, the date, time, length, where, self-diagnosis between these three groups, onset, offset, symptoms, and also my estimated heart rate. And some of them I was able to record with heart rate monitors, and then I looked at triggers. So by doing that, it was over three or four years, and this last year, then that I show here, I have depicted here in purple of the atrial fibrillation episodes. You can see they are 0 to 1, luckily not to many, but they are very bothersome. And then also supraventricular tachycardia, where it looked like it had some seasonality. And then I actually did a trial with some magnesium to see if it could decrease it. And it did decrease here, but I was a little bit skeptical about whether it was really due to the magnesium, because when I increased it later, the actual rate of them went up again. So it didn’t have an effect on atrial fibrillation, and the PSVT did go down, but there are all these other factors and wasn’t any kind of control. What about these triggers? And that was the thing that I really became interested in. And it could I quantify those triggers and could I use any epidemiologic methods from etiologic research like cancer to answer the question for myself. And there is something called from Murry Mittelman and Doctor MacClure, who I met and know; epidemiologists, a case-crossover design. And that’s a way to ask and answer the question, what were you doing right before you had the onset of disease, anything unusual at all. So in this kind of design, it’s really not that well known. You need to do a comparison within the individual. So I knew it would be perfect for me, because in this way I could compare what I was doing right before having an event, with what I usually do. And so you can actually have two comparisons. You can have one of what you’re doing on days when there is no events and what you’re doing on days when you do have the events. And so, you have a hazard and a control period, and then by doing this you can go ahead and use something called the odds ratio, and create a two by two table, to actually come up with quantified estimate of any kind of precipitant. So I went ahead and did that then for one year, and I found some interesting findings. And one of them was that high-intensity exercise had an odds ratio, so it’s four times greater risk than if I had that in the hour before than if I didn’t. I also found the interesting association with caffeine. 50 mg or more, after 2:00 PM, could really trigger these. That public meeting in large groups, I also found – and there is a lot of factors usually related to that, usually not getting enough sleep, of course catecholamine release all you know, stressors. But it really seemed like there was actually a big risk factor. And inadequate sleep in the previous 12 hours, so less than six hours sleep. The atrial fibrillation factors were very similar. But caffeine, it didn’t matter at what time of day it was. Usually, turbulence was a risk factor for me, so it always kind of bothered me and that’s a rare event, so that is a bigger odds ratio. And again I found the association with drinking wine, and public speaking in large groups and also inadequate sleep. But I don’t feel like I’m going to have one now, but that would be bad form if I collapsed here right on the stage today. So you know, the take-home message was that I use this information to minimize the precipitants, and I was able to decrease the number of all these episodes. And I ended up having three cardiologists that I work with, and they were very good about listening to what was going on, being able to tailor the kind of procedure that I ended up having. And I was really thankful for that, and I think that it helped that I had the information. And then I ended up having a far less evasive procedure, and just had a very easy ablation procedure for one of my arrhythmias, and then it knocked out all three of them. And so, my cardiologist said when I came back, then a month later, he said well, this is a home run Mark. And this is like the best possible scenario where we are able to ablate this atrial flutter which I had and I no longer get the other arrhythmias. So I would like to summarize this by saying that self-tracking, it helped me identify precipitating factors in a potentially life threatening heart condition. And I think single subject design as used by the Quantified Self components, you know far more study, validation, and publication and single subject design truly has a place in science and evidence-based medicine. And there’s methods available that can be expanded.
So with that, I would just like to thank you for your kind attention.
About the presenter[edit | edit source]
Mark Drangsholt gave this talk.